| 8:00 - 16:30
|
|
Registration
Grand Ballroom Foyer
|
| 8:35 - 9:15
|
|
Keynote 6: Epidemiology and Interventions
Grand Ballroom I + Parlors
Presenter:

|
Anna Wald, Professor
University of Washington, United States
Biography
Anna Wald, MD, MPH, Professor of Medicine, Epidemiology, and Laboratory Medicine & Pathology at the University of Washington and the Vaccine and Infectious Division, Fred Hutchinson Cancer Research Center, and Head of Division of Allergy and Infectious Diseases Division at the University of Washington. Dr. Wald co-directs the University of Washington’s Virology Research Clinic, which is a clinic dedicated to the study of epidemiology, natural history, and therapeutics for viral infections. Her research has focused on genital herpes infections, including infections in pregnant women and immunocompromised hosts. She has been an investigator in many clinical trials for novel antiviral agents, and prophylactic and therapeutic vaccines for HSV infection, as well as vaccines for HPV, CMV, and other viral pathogens. In the last few years, she has participated in multiple trials of therapeutic agents and investigational vaccines for SARS-CoV-2. Dr. Wald has been supported by NIH throughout her career. In addition to grants for scientific investigations, she has received a K24 Mentor Award from NIAID which supported the mentoring of the next generation of physician scientists.
|
Care for people with genital herpes
The care of people with HSV has not changed substantially in the last several decades. In today’s presentation, I will review the shortcomings of current therapies, difficulties with accurate diagnostics, persistent stigma, slow progress on vaccines and the potential for cure of HSV.
|
|
| 9:15 - 9:40
|
|
Symposium 6A: Epidemiology and Interventions
Grand Ballroom I + Parlors
Presenter:

|
Adriana Weinberg
Biography
Dr. Weinberg studied Medicine at the University of Sao Paulo, where she graduated first in her class both in Basic and Clinical Sciences. After residency, she completed an ID fellowship at Stanford University under the mentorship of Dr. Thomas Merigan. In 1990, Dr. Weinberg joined the faculty at the University of Colorado Denver School of Medicine to lead the Diagnostic Virology Laboratory of the Pediatric Infectious Diseases Section. She is currently a Tenured Professor of Pediatrics, Medicine and Pathology and Medical Director of the Clinical Molecular and Virology Laboratory at the University of Colorado Hospital.
Dr. Weinberg’s research has focused on immune protection against viral infections, including herpesviruses. She studies immune correlates of protection generated by vaccines and infections in immune competent and compromised hosts. Dr. Weinberg is the recipient of multiple federal and industry research grants that have supported her productive scientific career, which resulted in over 250 publications in peer-reviewed journals. Her work addresses both clinical and diagnostic aspects of herpesvirus infections. In recent years, this work focused mostly on correlates of immune protection against infections in immunocompetent and compromised children and adults - including infants, people living with HIV, transplant recipients and older adults. Dr. Weinberg’s research made seminal contributions to our understanding of the effect of age and immune senescence on responses to VZV and of the immunogenicity of both the live attenuated and the adjuvanted recombinant gE zoster vaccines.
|
IMMUNE RESPONSES TO SHINGLES VACCINES; CHANGING THE EPIDEMIOLOGY OF HERPES ZOSTER
Herpes zoster (HZ) is the clinical manifestation of varicella zoster virus (VZV) reactivation. Its incidence depends on the existence of latent VZV in sensory neurons and on the ability of the host cell-mediated immune (CMI) system to control the viral replication before symptoms ensue. Thus, the population at risk consists of people latently infected with VZV with weak CMI. Vaccines can decrease the incidence of HZ by reducing the prevalence of varicella and consequent VZV latency or by boosting the immune responses of latently infected hosts.
The recombinant zoster vaccine (RZV) prevents HZ in >90% of older vaccine recipients in the first 3 years and in >70% 10 years after immunization. These results elevate the RZV status to one of the most efficacious vaccines in older adults. We determined the immune response properties of RZV associated with its high efficacy. We determined that the persistent immunologic memory conferred by RZV is associated with recruitment of naïve CD4+ T cells into the immune response. We also showed that RZV is more likely to expand public clonotypes than other vaccines. Finally, we found evidence that RZV generates durable trained immunity that may contribute to protection against HZ.
|
|
| 9:40 - 10:05
|
|
Symposium 6B: Epidemiology and Interventions
Grand Ballroom I + Parlors
Presenter:

|
TingTing Wu
Biography
Ting-Ting Wu is an Associate Professor-in-residence of Molecular and Medical Pharmacology at University of California Los Angeles. She received her B.S. degree from National Taiwan University and earned her PhD from University of Pennsylvania, where she studied hepatitis delta virus and herpes simplex virus-1 with Dr. John Taylor. During her postdoctoral training in the laboratory of Dr. Ren Sun at UCLA, Dr. Wu focused on gammaherpesviruses, particularly MHV68 and KSHV. Together with Dr. Sun, she explored strategies of attenuating vaccine viruses by removing their ability to counteract the type I interferon (IFN-I). After setting up her independent research group at UCLA, Dr. Wu's work has centered on developing vaccine platforms for KSHV while investigating the molecular mechanisms by which the virus evades IFN-I. Since 2020, she has collaborated with Dr. Caius Radu at UCLA and Dr. Norbert Pardi at the University of Pennsylvania to enhance T cell responses elicited by mRNA vaccines. In addition to her research, Dr. Wu is the Director of the Graduate Program in Molecular Pharmacology Home Area at UCLA.
|
Our journey in KSHV vaccine development
Kaposi sarcoma-associated herpesvirus (KSHV), linked to several malignancies and serious illnesses, is highly prevalent in Africa where it primarily causes Kaposi sarcoma (KS). Our team is committed to developing a vaccine to reduce or eliminate the risk of KSHV-related diseases significantly. Over the years, we have explored various vaccine platforms, such as live attenuated viruses, non-infectious virus-like vesicles (VLVs), and subunit-based strategies. In collaboration with Dr. Sun's laboratory, we have created latency-deficient, severely attenuated recombinant viruses that elicit strong immune responses and provide effective protection, as demonstrated using the closely related rodent virus, MHV-68.
Our research on non-infectious KSHV VLVs has led to the discovery of a novel complement-mediated immune mechanism for neutralizing KSHV. Additionally, we are working with Dr. Hong Zhou's laboratory at UCLA to characterize the structure of an essential KSHV glycoprotein involved in viral fusion during entry. This structural knowledge is crucial for designing effective antigens to stimulate neutralizing antibodies.
Recently, we have been working towards developing mRNA vaccines and lipid nanoparticle-based adjuvants in collaboration with Dr. Radu's laboratory at UCLA and Dr. Pardi's laboratory at UPenn, along with Acuitas Therapeutics. These collaborations are pivotal as they aim to elicit robust T-cell and antibody responses through our subunit-based vaccines. By integrating innovative vaccine platforms and adjuvants with our antigen designs, we are dedicated to establishing robust immunization strategies against KSHV.
|
|
| 10:05 - 10:30
|
|
Symposium 6C: Epidemiology and Interventions
Grand Ballroom I + Parlors
Presenter:

|
Karen Fowler, Professor
University of Alabama at Birmingham, United States
Biography
Karen Fowler is a Professor of Pediatrics in the Division of Pediatric Infectious Diseases at the University of Alabama at Birmingham. Her research has focused on the epidemiology, natural history, and pathogenesis of maternal and congenital cytomegalovirus infections and the role of congenital CMV infection in sensorineural hearing loss in children. She is also interested in evaluating whether social determinants may be contributing to the disparities seen in HCMV infection rates and could identify the subset of HCMV seropositive women who are at increased risk of in utero transmission of the virus. She was the Co-Director of the NIDCD-funded CHIMES Study, which screened and enrolled over 12,000 infants at UAB and 100,000 infants nationally. Her current NIH grant is recruiting young pregnant women in Jefferson County prenatal health clinics into a 12-week cognitive-behavioral intervention to increase knowledge about HCMV, decrease self-reported risk behaviors, and demonstrate reduced primary and nonprimary maternal HCMV infections during pregnancy. Dr. Fowler serves on the scientific advisory committee for the National CMV Foundation and received the National CMV Foundation Professional Impact Award in Fall 2023.
|
Maternal and Congenital Cytomegalovirus Infections: Epidemiology and Interventions
Congenital CMV infection (cCMV) is found worldwide. It contributes to thousands of children each year being born with or developing permanent disability such as hearing loss, vision loss, cerebral palsy, and cognitive impairment. The cCMV landscape in the US is changing with the expansion of targeted and universal newborn CMV screening in hospitals and states. An increased number of infants being identified with cCMV will contribute to our understanding of the epidemiology of cCMV. Although we know what factors contribute to CMV acquisition among women of childbearing age, we do not know which of the women will deliver a newborn with cCMV. Both women with a primary infection during pregnancy and seroimmune women can deliver a newborn with cCMV infection. Vaccine development has primarily focused on preventing primary infection in pregnancy. Eliminating primary infections could reduce the disease burden due to cCMV, but CMV-related sequelae caused by nonprimary infections would remain. Although vaccine strategies are promising, currently, there are no CMV vaccines on the market to prevent CMV infection in pregnant women. In the meantime, CMV prevention interventions are being explored. Due to the lack of CMV awareness in women, any CMV prevention intervention must include some educational awareness before discussing how to reduce risk behaviors since most women are unaware of CMV and CMV risk behaviors. Also, prevention strategies must consist of prevention for both primary and nonprimary maternal CMV infections to decrease the incidence and disease burden of cCMV infection successfully. We have an ongoing CMV behavioral intervention clinical trial in a high-risk, primarily seropositive pregnant population. Our study assesses whether a behavioral intervention is feasible and acceptable, whether their knowledge about CMV and cCMV risks increases, and whether increased knowledge and behavior change lowers seroconversions and nonprimary CMV infections during pregnancy.
|
|
| 10:30 - 11:00
|
|
Refreshment Break
Pavillion Ballroom & Foyer
|
| 11:00 - 12:30 - Concurrent Session
|
|
Session 4A: Epidemiology and Interventions
Galleria
|
|
Session 4B: Virus Host Interactions
Grand Ballroom I + Parlors
|
|
Session 4C: Gene Expression
Grand Ballroom II
|
| 12:30 - 13:30
|
|
Lunch
Pavillion Ballroom & Foyer
|
| 12:45 - 13:30
|
|
IHW Organizational Meeting
Galleria
|
| 13:30 - 14:10
|
|
Keynote 7: Evolution, Genomics, Systems Biology
Grand Ballroom I + Parlors
Presenter:

|
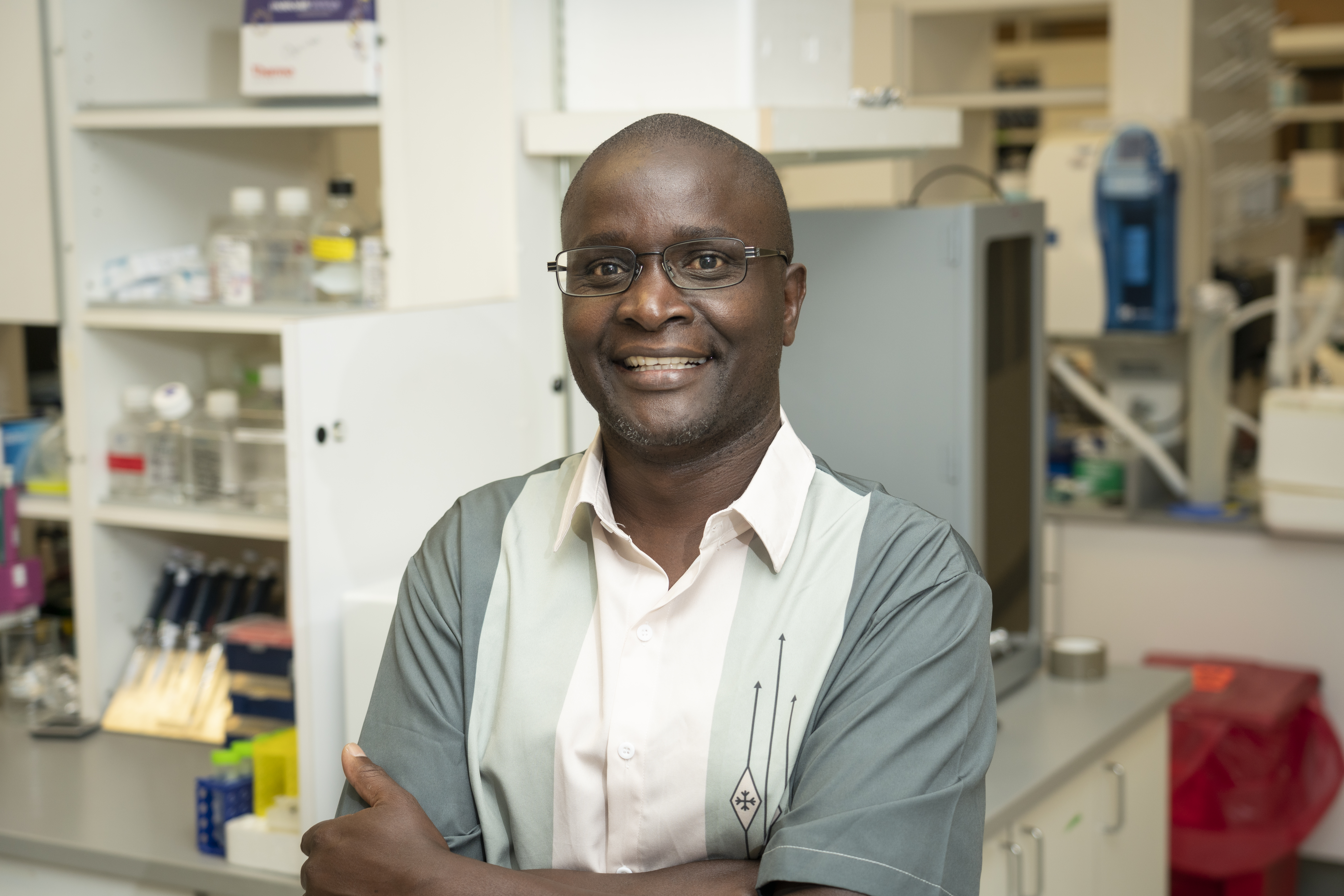
Charles Wood, Cancer Crusader Professor
Louisiana State University Health Sciences Center- New Orleans, United States
Biography
Dr. Charles Wood is Cancer Crusader Professor of the Department of Interdisciplinary Oncology at the Louisiana State Health Sciences Center- New Orleans, and Associate Director of Basic Research at the Stanely Scott Cancer Center. His significant academic and administrative experience includes serving as the director of a research center, as the principal investigator (PI) and Co-PI of several active multi-center and multi-national collaborative projects. He joined LSU-Health from the University of Nebraska, where he held the University Professorship, and was founding director of the Nebraska Center for Virology in 2000, a COBRE supported center that spans the entire University of Nebraska system forming the first research network throughout the state.
Dr. Wood leads research collaborations and exchanges between different partners in Africa and the LSUSHC. Dr. Wood began his research on HIV/AIDS in sub-Saharan Africa more than 29 years ago in Zambia. These research programs have been expanded to Tanzania with support from the National Institute of Health. He currently directs an active NIH-funded research team studying HIV and Kaposi sarcoma, and KS associated human herpesvirus. He is deeply committed to the training and development of the next generation of undergraduate and graduate students, and researchers. He also served as Director of two NIH Fogarty International Training and Research Programs, with a focus on HIV research and training of the next generation of graduate students and post-graduate researchers in Zambia, and more recently in Tanzania.
|
What we learned about the Kaposi Sarcoma associated herpesvirus in sub-Saharan Africa
Kaposi’s Sarcoma (KS) is a highly prevalent malignancy in sub-Saharan Africa (SSA), especially in HIV-1 infected individual even in the era of anti-retroviral therapy (ART), and KS remains the one of the most common cancers in the SSA population, especially in men. The etiologic agent of KS is Kaposi’s sarcoma-associated herpesvirus (KSHV) or human herpesvirus-8 (HHV-8), and the high incidence of KS parallels the high prevalence of KSHV infection in SSA. Our team has a long-standing research program in understanding KSHV transmission and KS disease pathogenesis in SSA. Studies from our laboratory, and others indicate that KSHV seroprevalence can range between 50-90% in SSA. We have also elucidated the mechanisms and risk factor of KSHV transmission. We found KSHV infection occurred mostly during early childhood in SSA, it was transmitted mainly via saliva contact with HIV-1 infection and immunosuppression as major risk factors. Thus, there is a need to better understand the immune response against the virus in order to prevent infection and the development of KS in KSHV infected individuals. We have recently demonstrated the utility of phage display technique – VirScan coupled to PhIP-seq, in facilitating the first high-resolution linear epitope mapping of the KSHV proteome to date. Consistently targeted epitopes in both KS and asymptomatic individuals in SSA subjects resided in several immunodominant proteins. Using unbiased machine-learning, reactivity to a subset of viral peptides were able to distinguish KS patients from asymptomatic individuals. Therefore, this approach is currently being used to expand the model to encompass the humoral responses against the human virome. Elucidation of antibody repertoires is vital to discerning host-pathogen interactions, establishing biomarkers for early detection and progression of disease, as well as designing effective vaccine and therapeutic strategies.
|
|
| 14:10 - 14:35
|
|
Symposium 7A: Evolution, Genomics, Systems Biology
Grand Ballroom I + Parlors
Presenter:

|
John Purdy, Associate Professor
Immunobiology, University of Arizona, United States
Biography
IHW 2024 in Portland is a trip home for John Purdy. He is an Oregonian at heart, particularly during the beautiful summer months. His undergraduate degree is from Pacific University in Forest Grove on the western edge of the Portland Metro area. After completing a PhD at Penn State College of Medicine in Hershey PA, John moved to Princeton University to do postdoctoral research in metabolism with Dr. Joshua Rabinowitz. While at Princeton he wandered into Dr. Thomas Shenk’s laboratory and emerged several years later as a herpesvirologist. While he grew up harvesting marionberries and chasing cattle on a farm an hour south of Portland, he now spends his time harvesting human cytomegalovirus stocks and chasing after novel ideas related to virus-host metabolism interactions. His research investigates how viruses hijack host metabolism to support their replication and how the host uses metabolism to limit viruses. John is currently an Associate Professor in the Department of Immunobiology and the BIO5 Institute at the University of Arizona. He is an editorial board member for the Journal of Virology, a founding member of the ASV DEI Committee, co-author of a chapter in Fields Virology with Dr. James Alwine, presented as State-of-the-Art lecture at ASV 2022 conference, and has performed ad hoc service on several NIH Study Sections.
|
Understanding Metabolic Dynamics at the Virus-Host Interface following HCMV Infection
From entry into and exit from cells, the replication of herpesviruses requires metabolism. Since herpesviruses do not encode a metabolic network, successful virus infection depends on host metabolism. We focus on human cytomegalovirus (HCMV), a common herpesvirus that causes disease in the immunocompromised and is a leading cause of congenital disabilities. Our research defines the virus-host metabolism interactions that aid HCMV to successfully replicate, specifically changes in lipid metabolism. We demonstrated that HCMV infection promotes lipid synthesis, altering the host lipidome to establish a lipid environment that favors virus replication. Moreover, a virus's dependency on host metabolism is a weakness the host can exploit—or potentially scientists—to restrict virus replication. A more recent theme of our research is to understand how host cells regulate metabolism to reduce virus replication, i.e., metabolism as an intrinsic cellular antiviral defense. Overall, our studies reveal the dynamics between the host and HCMV in raising or lowering a metabolic barrier during virus replication.
|
|
| 14:35 - 15:00
|
|
Symposium 7B: Evolution, Genomics, Systems Biology
Grand Ballroom I + Parlors
Presenter:

|
Daniel Malouli, Research Assitant Professor
Oregon Health & Science University, United States
Biography
For his undergraduate education, Dr. Malouli enrolled in a biochemistry program jointly offered by the Leibniz University of Hannover, the University of Veterinary Medicine Hannover (TiHo) and the Hannover Medical School (MHH) in Hannover, Germany. After rotating in different virology laboratories in Germany, Ireland and the USA, he joined the group of Prof. Dr. Martin Messerle at the Hannover Medical School (MHH) for his master's degree to work on a CD8+ T-cell immune evasion mechanism of the murine cytomegalovirus (MCMV). Subsequently, he moved to Portland, Oregon to perform his graduate work on the molecular characterization of the rhesus cytomegalovirus (RhCMV) and the development of attenuation strategies for CMV based vaccine vectors at the OHSU Vaccine and Gene Therapy institute under the supervision of Prof. Dr. Klaus Früh. After receiving his Ph.D. from the Leibniz University of Hannover, Dr. Malouli joined the laboratory of Prof. Dr. Louis Picker at the VGTI as a staff scientist to study how RhCMV modulates the host CD8+ T-cell response and to optimize the design of CMV based vaccine vectors for pre-clinical and clinical studies. In 2018, he was promoted to research assistant professor and invited to start his own research group as part of the VGTI faculty. His laboratory has focused on modelling HCMV infection biology and pathology in relevant NHP models using model specific NHP-CMV species to further our understanding of CMV in vivo behavior and to establish a model system that can be used to interrogate novel vaccine and interventions approaches.
|
Using NHPs to study CMV pathogenesis and immunomodulation in relevant and predictive in vivo animal model systems.
Cytomegaloviruses (CMVs) are widespread pathogens that have been isolated from various rodent and primate species. All examined CMVs encode for upwards of 200 individual viral proteins that can reshape the cellular environment in the infected host to benefit virus replication and enable persistence. Due to its strict species-specificity, human CMV (HCMV) does not productively replicate in any immunocompetent animal model. Thus, CMVs specific for the laboratory animals used have to be employed to study virus/host interactions in vivo. Among the usable laboratory animal species, non-human primates (NHPs) infected with NHP CMVs represent the evolutionary closest and thus potentially most predictive model to study HCMV infections. Prior research has demonstrated that many aspects of HCMV pathogenesis are recapitulated in rhesus macaques (RM) infected with rhesus CMV (RhCMV). Thus, we examined the contribution of proteins involved in viral tropism and dissemination initially identified and characterized in HCMV tissue culture models but functionally conserved across primate CMVs. Intriguingly, infections of CMV naïve RM demonstrated that in vivo tropism and dissemination differs from observations in tissue culture models. We furthermore applied the RM model to identify and characterize highly unconventional and unique cellular immune responses induced by the virus against itself and any introduced foreign antigen. Vaccine vectors based on CMV have demonstrated unprecedented protection from SIV challenge. We have now identified a genomic locus in NHP CMVs that determines species specificity of these responses. This information could allow us to generate HCMV vectors that can be evaluated for efficacy in vivo in a relevant animal model. Combined, our results indicate that NHPs can serve as a valuable and predictive model to study CMV immunology and pathogenesis in vivo and to interrogate virus/host interactions deemed valuable intervention and vaccine targets to inform drug and vaccine development prior to translation to human clinical trials.
|
|
| 15:00 - 15:30
|
|
Refreshment Break
Pavillion Ballroom & Foyer
|
| 15:30 - 16:10
|
|
Bernard Roizman Lecture
Grand Ballroom I + Parlors
Presenter:
|
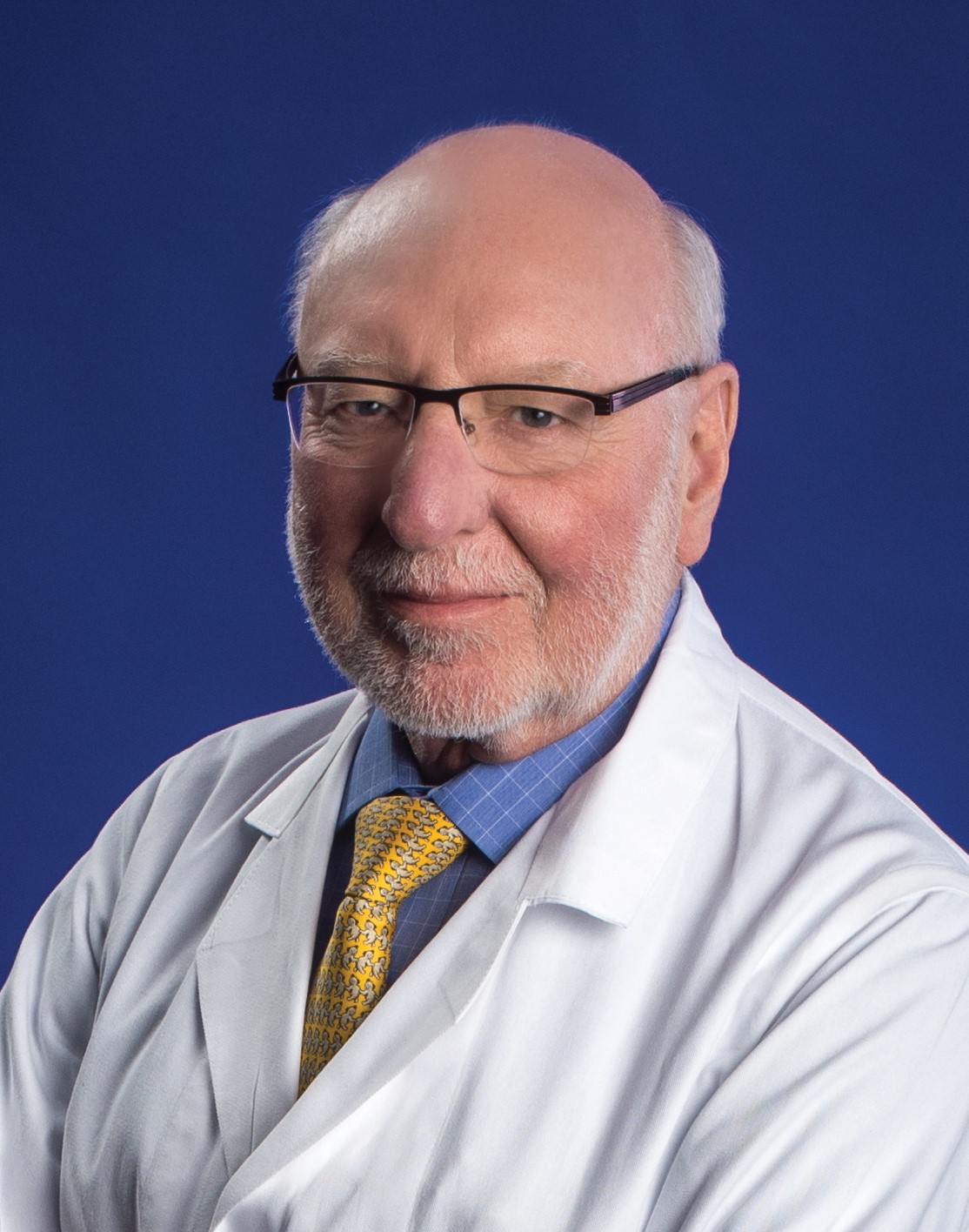
Richard Whitley
Biography
Dr. Richard Whitley is a Distinguished Professor of Pediatrics, Vice Chairman for Research in the Department of Pediatrics and Co-Division Director of Pediatric Infectious Diseases at the University of Alabama at Birmingham School of Medicine. He also holds the titles of Loeb Eminent Scholar Chair in Pediatrics; Professor of Microbiology, Medicine, & Neurosurgery; Senior Scientist, Department of Gene Therapy; Co-Founder, Alabama Drug Discovery Alliance, and Associate Director, Drug Discovery and Development, Comprehensive Cancer Center.
An expert on how antiviral therapies fight infections in children and adults, Dr. Whitley’s research spans four decades, during which he has published 401 scholarly articles on pediatric infectious disease. In 2019, Dr. Whitley was appointed by Dr. Anthony Fauci to chair the NIH-NIAID COVID-19 Data Safety and Monitoring Board. Today, he continues to serve as a member of the Steering Committee for the NIH Long COVID-RECOVER initiative.
After attaining his medical degree from George Washington University School of Medicine in 1971, Dr. Whitley completed his pediatric internship/residency and fellowship in infectious disease and virology at UAB from 1971 to 1976. Dr. Whitley’s honors are numerous and his professional organization involvement extensive, including NIAID AIDS Task Force membership; NIAID DSMB Clinical Trials Committee (Chairman); Associate Editor, Journal of Infectious Diseases (2005-Present); President, International Society for Antiviral Research (1988-1990); AAP Award for Excellence in Pediatric Research (1991); Elion Award, International Society for Antiviral Research (2004); Chair, BSC, CCID, CDC (2005-2010), UAB President’s Medal (2007), NIH National Adv Allergy and Infectious Disease Council (2008-2012), and President, Infectious Diseases Society of America (2009). In 2013, he was named as the inaugural recipient of the Distinguished Clinical Research Scholar and Educator in Residence at the NIH Clinical Center. He has received numerous other awards and lectureships, including the 2016 UAB SOM Dean’s Excellence Award in Research for Senior Faculty, the Department of Pediatrics Lifetime Achievement Award in Pediatric Healthcare in 2016, and Honorary Fellowship of the Royal College of Physicians of Ireland, Irish Academy of Medicine in 2018. Dr. Whitley received the Alexander Fleming Award for Lifetime Achievement from the Infectious Diseases Society at their annual meeting in 2018. He received the 2020 National Foundation for Infectious Diseases John P. Utz Leadership Award for his work in the field of clinical virology in December 2020, and in 2022, he received the John Howland Award from the American Pediatric Society.
|
The History and Status of Oncolytic Herpes Simplex Virus
While most herpes simplex virologists are familiar with studies using herpes simplex virus (HSV) to treat melanomas and experimentally to determine potential beneficial effects upon administration directly into glioblastomas (GBM), few know the origin of such studies. The work leading to the development of oncolytic HSV began with an NIH/NCI Program Project Grant evaluating latency and neurovirulence. From neurovirulence studies, virus obtained from patients with herpes simplex encephalitis by biopsy were more neurovirulent that lip isolates from the same individual when inoculated directly into the mouse brain. This finding led to transfections of virulent into avirulent virus with sequencing and the identification of the 134.5 gene. Deletion of 134.5 resulted in an avirulent virus upon direct inoculation into the mouse brain but remained replication competent in dividing cells.
This observation led to the first Phase 1 clinical trial with G207 (originating from the Matuza and Weller laboratory) in patients who had failed standard therapy of GBM, being performed at Georgetown University and University of Alabama at Birmingham (UAB) that established safety and led to a dose escalation study, suggesting prolonged survival in some volunteers but no cures.
In parallel, studies in children with refractory GBM were performed at UAB. These studies unequivocally demonstrated prolonged survival in children undergoing direct convection delivery of virus into the tumor bed. However, again there were no survivors.
In parallel, Amgen studied a similar virus (TEVEC) for patients with melanoma; ultimately resulting in its licensure. Treatment studies of GBM, however, continued with the development of a virus that expresses IL-12. This study was recently completed by Markert at UAB. An IL-2 and PD-1 expressing virus has gone into clinical trials both in China and in the United States.
The date from these studies will be summarized and updated.
|
|
| 15:30 - 16:30
|
|
Handover
Grand Ballroom I + Parlors
|
| 18:00 - 23:30
|
|
Banquet at the Portland Art Museum
Offsite
|
 Remembering Jay Nelson
Remembering Jay Nelson








.jpg)